What Exactly is PCOS?
Polycystic Ovary Syndrome (PCOS) is one of the most common hormonal disorders that affects women of reproductive age. Simply put, it happens when your ovaries produce more androgens (male hormones) than they should, which throws off the balance of your reproductive system. This can make your periods irregular, cause you to gain weight unexpectedly, or even lead to fertility issues. But don’t worry—PCOS is not the end of the world, understanding PCOS help you have more advantage in managing your fertility journey, and there are ways to manage it! You’re not alone in this, as millions of women around the world are navigating their PCOS journey, and you can too.
You might be wondering: why does this happen? While the exact cause of PCOS is still a bit of a mystery, experts believe that genetics, insulin resistance, and inflammation play key roles. If your mom or sister has PCOS, there’s a higher chance you might develop it as well. It’s like getting the family recipe no one asked for. But instead of a cake recipe, it’s a hormone imbalance that can affect your health in different ways.
Recognizing the Symptoms of PCOS
The symptoms of PCOS can vary greatly from one person to another, which makes it a bit tricky to recognize. Some women experience just one or two symptoms, while others might deal with several. It’s like your body is playing a game of roulette—sometimes it’s light, and other times it’s full-on. The most common symptom is irregular periods, which can be annoying when you’re trying to track your cycle or plan a pregnancy. You might notice your periods come less frequently, or in some cases, you might go months without having one at all. This is because ovulation either stops or happens infrequently in women with PCOS.
Another key symptom is weight gain, particularly around the belly. If you feel like no matter how much you exercise or watch what you eat, the weight just won’t budge, PCOS could be the culprit. This happens because many women with PCOS have insulin resistance, which can cause the body to store more fat, especially around the midsection. It’s frustrating, but once you know what’s going on, it’s easier to tackle.
The Not-So-Fun Hair Growth (Or Loss)
One of the more noticeable symptoms of PCOS is hirsutism—excess hair growth in places you wouldn’t typically expect, like your face, chest, or back. This happens because those elevated androgen levels stimulate hair growth in areas where men usually grow hair. If you’ve been plucking, waxing, or shaving more than usual, PCOS could be the reason behind it. And on the flip side, while some parts of your body may experience hair growth, your scalp might experience hair thinning or loss, a condition called androgenic alopecia. This can be a frustrating double whammy, but knowing it’s linked to PCOS can help you get the right treatment.
Click here to learn more about Androgenic alopecia
Acne and Skin Changes
Many women with PCOS also deal with acne, especially on the lower part of the face, like the jawline and chin. This isn’t the occasional pimple either—it can be persistent, and often stubborn to treat. The high levels of androgens stimulate the production of oil in the skin, leading to clogged pores and, unfortunately, breakouts. You might feel like you’re stuck in a teenage nightmare with breakouts that just won’t quit. And then there’s the issue of dark patches of skin, particularly around the neck, armpits, or under the breasts. This condition, called acanthosis nigricans, can be a sign of insulin resistance, which is common in women with PCOS.
Fertility Challenges
One of the most significant concerns for women with PCOS is fertility. If you’ve been trying to conceive and aren’t seeing those two little lines on a pregnancy test, PCOS could be playing a role. When ovulation doesn’t happen regularly, it can be difficult to pinpoint your fertile window. In some cases, ovulation stops altogether, making conception even more challenging. But here’s the good news: while PCOS can make it harder to get pregnant, it doesn’t make it impossible. Treatments like medication to induce ovulation, lifestyle changes, and fertility treatments like IVF can help. Many women with PCOS go on to have healthy pregnancies and beautiful babies.
Mood Swings and Fatigue
Aside from the physical symptoms, PCOS can also take a toll on your mental health. It’s not uncommon to feel mood swings, anxiety, or depression as a result of the hormonal imbalances happening in your body. Fatigue is another symptom that often goes hand-in-hand with PCOS. If you feel like you’re constantly dragging, even after a good night’s sleep, your hormones might be to blame. The combination of irregular blood sugar levels, weight struggles, and dealing with physical symptoms can leave you feeling exhausted.
Common Fertility Challenges with PCOS
Polycystic Ovary Syndrome (PCOS) is one of the leading causes of infertility in women, but don’t lose hope! Even though PCOS can make it harder to conceive, many women with this condition do go on to have successful pregnancies. The key is understanding the fertility challenges PCOS presents, so you can work with your doctor on finding the best solution for you. Let’s dive into the most common fertility struggles women with PCOS face and how to overcome them.
Irregular Ovulation: The Biggest Roadblock

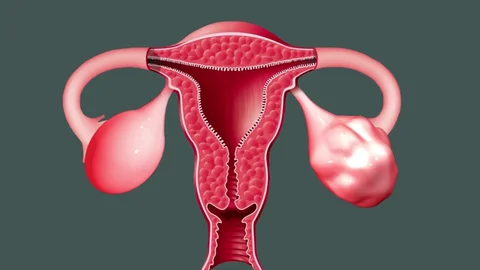
One of the main reasons women with PCOS struggle to get pregnant is irregular ovulation—or sometimes, no ovulation at all. Ovulation is the process where your body releases an egg, giving it the chance to meet sperm and make magic happen (a.k.a. conception). However, with PCOS, your ovaries don’t always play by the rules. You might ovulate less frequently, or in some cases, you might not ovulate at all.
Why does this happen? The hormonal imbalance caused by PCOS, particularly the excess of male hormones (androgens), disrupts your body’s normal ovulation process. Without regular ovulation, your menstrual cycle becomes irregular, and it’s hard to predict your most fertile days. If you’re trying to conceive, this can make things frustrating. But the good news? There are treatments available to help jump-start ovulation, so all hope is not lost!
Hormonal Imbalances and Their Effects
With PCOS, your body’s hormone levels are often out of whack, and this can wreak havoc on your fertility. The imbalance of androgens and insulin (a hormone that controls blood sugar) leads to a whole host of fertility issues. Insulin resistance is common in women with PCOS, meaning your body struggles to use insulin properly. This causes your body to produce more insulin than it needs, which in turn leads to higher androgen levels. And, unfortunately, those high androgen levels prevent your ovaries from releasing an egg regularly.
When your hormones are out of balance, everything from ovulation to egg quality can be affected. Sometimes, your body produces too many small, immature follicles (those little fluid-filled sacs in the ovaries), but none of them develop into a mature egg. Without a mature egg, fertilization simply can’t happen. While this sounds like a lot to deal with, medications like clomiphene or letrozole can help regulate hormone levels and get ovulation back on track.
Weight Gain and Insulin Resistance
Weight gain is a common symptom of PCOS, and it’s closely linked to insulin resistance. Unfortunately, this can create a vicious cycle when it comes to fertility. Extra weight—especially around the abdomen—can make your body even more resistant to insulin, which in turn exacerbates the hormonal imbalances that disrupt ovulation. It’s a bit like your body is stuck in a loop, and the more weight you gain, the harder it is for your fertility to function properly.
The good news? Even modest weight loss (as little as 5-10% of your body weight) can significantly improve ovulation and boost your chances of conceiving. If you’re dealing with weight gain and PCOS, a combination of a balanced diet and regular exercise can help manage insulin resistance and improve your fertility. It doesn’t mean you have to become a gym fanatic—small, sustainable changes can make a big difference over time.
Difficulty with Implantation
In some cases, women with PCOS face challenges not just with ovulation, but with implantation too. Even if you’re able to release a healthy egg and it meets sperm, the fertilized egg may struggle to implant in your uterus. The thickening of the uterine lining—usually caused by those pesky hormone imbalances—can make it harder for the embryo to stick and grow. This can be frustrating and emotional, especially if you’ve been trying to conceive for a while.
This is why regular monitoring and working with a fertility specialist is so important. They can help you manage your cycle and ensure that your body is ready for pregnancy. For some women with PCOS, fertility treatments like IVF (in vitro fertilization) may be necessary to bypass these challenges, but many still have successful pregnancies through less invasive methods like ovulation-inducing medications. PCOS and fertility
Emotional and Mental Struggles

Fertility struggles don’t just affect your body—they can take a toll on your mental and emotional well-being too. Dealing with PCOS and infertility can be stressful, and it’s completely normal to feel overwhelmed. The pressure of tracking ovulation, managing symptoms, and waiting for that positive pregnancy test can lead to anxiety and frustration. It’s important to give yourself grace and remember that you’re not alone in this journey.
Finding a support system—whether it’s through friends, family, or a fertility group—can help you navigate the emotional ups and downs. And don’t forget to take care of yourself outside of fertility treatments! Whether it’s practicing yoga, going for a walk, or simply taking time to relax, finding ways to manage stress can make a big difference in your overall health and fertility journey.
Treatment Options for PCOS-Related Infertility
Polycystic Ovary Syndrome (PCOS) is one of the most common causes of infertility in women, but the good news is that it’s treatable! If you’ve been diagnosed with PCOS and are struggling to get pregnant, there are plenty of treatment options that can help. From lifestyle changes to fertility medications and advanced treatments like IVF, you’ve got several paths to explore. Let’s break down the options so you can find what might work best for your body and your baby-making journey.
Lifestyle Changes: Your First Line of Defense
Sometimes, the first step toward treating PCOS-related infertility is as simple as making some lifestyle adjustments. If you’re dealing with PCOS, you’ve likely heard about the importance of managing your weight, and for good reason. Weight gain, especially around your abdomen, can exacerbate insulin resistance, which is closely tied to PCOS. But here’s the good news: you don’t need to lose a lot of weight to see big improvements. Even a modest weight loss of 5-10% can help regulate your menstrual cycle and improve ovulation. So, if you’re aiming for a healthier lifestyle, think about small, sustainable changes rather than a full-blown overhaul.
A balanced diet and regular exercise can go a long way in managing insulin levels and hormone imbalances. Focus on whole foods like fruits, veggies, lean proteins, and healthy fats. Cutting back on refined carbs and sugary snacks can help, too. But remember—this isn’t about restrictive dieting. It’s about giving your body the fuel it needs to function properly. And don’t forget about exercise! Whether it’s a daily walk, yoga, or a light workout, keeping your body moving can improve your overall fertility health.
Ovulation Induction: Jump-Starting Your Cycle
One of the biggest fertility challenges with PCOS is irregular ovulation, or in some cases, the absence of ovulation altogether. Fortunately, there are medications available to help your body ovulate more regularly, a process known as ovulation induction. The most commonly prescribed medications are Clomiphene Citrate (Clomid) and Letrozole (Femara), both of which work by encouraging your ovaries to release a mature egg.
Clomiphene has been the go-to fertility medication for years and works by blocking estrogen receptors, tricking your brain into producing more follicle-stimulating hormone (FSH). This increase in FSH stimulates your ovaries to release an egg. Letrozole, on the other hand, is actually a medication used to treat breast cancer, but it’s shown great success in women with PCOS by lowering estrogen levels and prompting ovulation. If one medication doesn’t work, don’t get discouraged—sometimes it takes a little trial and error to find the right solution.
The process of ovulation induction typically involves taking medication early in your cycle and being monitored via ultrasound to track your progress. It might feel like a lot at first, but many women with PCOS see great results from these medications, helping them get one step closer to that positive pregnancy test.
Metformin: Tackling Insulin Resistance
If your PCOS is linked to insulin resistance (which is common), your doctor might suggest Metformin as part of your treatment plan. Metformin is a medication traditionally used to treat type 2 diabetes, but it’s also incredibly helpful in regulating insulin levels for women with PCOS. By improving how your body uses insulin, Metformin can help lower androgen levels and, in turn, improve ovulation.
One of the best things about Metformin is that it tackles multiple symptoms at once. Not only can it help restore regular ovulation, but it may also assist with weight management and reduce the risk of developing type 2 diabetes down the road. However, it’s important to note that Metformin isn’t a magic fix for everyone, and it’s often used in conjunction with other treatments like ovulation induction. you can also read more on PCOS and fertility related topics here.
In Vitro Fertilization (IVF): A More Advanced Option
If lifestyle changes and medications don’t seem to be working, In Vitro Fertilization (IVF) could be your next step. IVF is a more advanced fertility treatment, but it’s often a game-changer for women with PCOS who haven’t had success with less invasive methods. With IVF, your ovaries are stimulated to produce multiple eggs, which are then retrieved and fertilized in a lab. The resulting embryos are carefully monitored, and the healthiest one is transferred back into your uterus, where it hopefully implants and results in a pregnancy.
IVF can sound a bit intimidating (and it can be pricey), but it’s also one of the most effective treatments available, especially for women dealing with ovulation disorders like PCOS. The controlled environment of IVF allows your doctor to closely monitor egg development, fertilization, and embryo quality, giving you a higher chance of success. Many women with PCOS find that IVF gives them the best shot at achieving their dream of becoming a parent, even after other treatments haven’t worked.
Fertility-Friendly Medications and Procedures
Sometimes, doctors might suggest a combination of fertility treatments to improve your chances of conceiving. In addition to ovulation-inducing medications, Intrauterine Insemination (IUI) is another option. This is a less invasive procedure where sperm is placed directly into your uterus to increase the chances of fertilization. IUI can be combined with medications like Clomiphene or Letrozole to help time the insemination with your ovulation cycle.
Another fertility-friendly treatment you may encounter is Ovarian Drilling—a laparoscopic procedure where small holes are made in the surface of your ovaries to reduce androgen production and promote ovulation. While it sounds a bit intense, it’s actually a minimally invasive procedure and is used when medications alone haven’t worked.
PCOS and Fertility: How Lifestyle Changes Can Manage PCOS
Polycystic Ovary Syndrome (PCOS) can feel like an overwhelming condition to manage, but the good news is that simple lifestyle changes can make a big difference. While there isn’t a cure for PCOS, taking control of your daily habits can help reduce symptoms, improve your overall health, and even increase your chances of conceiving. The key is to focus on small, sustainable changes that fit into your routine. Let’s explore how these changes can help you manage PCOS and feel more in control of your body.
Balanced Diet: Nourishing Your Body the Right Way

A healthy, balanced diet is one of the most important factors in managing PCOS. With PCOS, your body may struggle with insulin resistance, which can lead to weight gain and further hormone imbalances. Eating a diet that’s rich in whole foods like vegetables, fruits, lean proteins, and healthy fats can help regulate your blood sugar levels and reduce the impact of insulin resistance.
Start by incorporating more fiber into your meals. Foods like oats, beans, and leafy greens are packed with fiber, which can help slow down digestion and keep your blood sugar levels steady. You don’t need to cut out carbs entirely, but try to avoid refined carbohydrates like white bread and sugary snacks. Instead, choose whole grains like quinoa and brown rice. Small swaps like these can make a big impact over time.
Healthy fats are also a must. Omega-3 fatty acids, found in foods like salmon, walnuts, and flaxseeds, can help reduce inflammation, which is often a concern for women with PCOS. Remember, it’s not about depriving yourself—it’s about nourishing your body with the right fuel so it can function at its best.
Exercise: Moving Your Body to Manage Symptoms
Exercise is another powerful tool in managing PCOS. Regular physical activity can help with weight management, improve insulin sensitivity, and reduce androgen levels (those pesky male hormones that tend to be elevated in women with PCOS). But don’t worry—you don’t have to hit the gym seven days a week to see results.
In fact, even moderate exercise can have a huge impact on your overall health. Activities like walking, swimming, yoga, or cycling are great options for staying active without overloading your body. Aim for about 30 minutes of exercise most days of the week, but listen to your body and find what works for you.
Strength training can also be particularly beneficial for women with PCOS. Building muscle helps improve your body’s sensitivity to insulin and supports a healthy metabolism. Plus, you’ll feel stronger and more empowered along the way! Whether it’s lifting light weights or doing bodyweight exercises at home, strength training is a great way to complement your fitness routine.
Managing Stress: Prioritizing Your Mental Health
It’s easy to overlook the impact that stress has on PCOS, but managing stress is just as important as eating right and exercising. High levels of stress can lead to elevated cortisol levels, which can worsen insulin resistance and hormone imbalances. So, finding ways to manage stress is crucial for your overall well-being.
Meditation, deep breathing exercises, or even taking a few minutes each day for yourself can help reduce stress levels. Mindfulness activities like yoga or journaling can also give you a much-needed break from the hustle and bustle of daily life. Don’t feel guilty about taking time to relax—it’s an essential part of managing your health.
Sleep is another big factor in managing stress and PCOS symptoms. Aim for 7-9 hours of quality sleep each night. A good sleep routine can help regulate your hormones and improve your mood. Make sure to wind down before bed, avoid screens for at least an hour before sleeping, and create a calming bedtime environment. Good sleep hygiene can make a huge difference in how you feel.
Consistency Over Perfection: Small Changes Make a Big Impact
Managing PCOS through lifestyle changes doesn’t mean you have to be perfect every day. The key is consistency over time. Even small, gradual changes in your diet, exercise routine, and stress management can add up to significant improvements in your symptoms. Don’t stress about making drastic changes overnight—it’s about finding what works for you and sticking with it.
Remember, every little step you take toward a healthier lifestyle brings you closer to managing your PCOS more effectively. Celebrate your progress, whether it’s adding more veggies to your meals, going for a walk, or simply taking a moment to breathe and relax. You’ve got this!
Takeaway: Empowering Yourself with Lifestyle Changes
PCOS can be challenging, but it doesn’t define you. By making small, manageable lifestyle changes, you can take control of your symptoms and improve your overall quality of life. A balanced diet, regular exercise, stress management, and good sleep habits are all key tools in your PCOS toolkit. It’s not about perfection, but about finding balance and being kind to yourself as you work toward a healthier you. Give our fertility expert team a go, we make sure we get you your desired result all the time.
So, whether you’re just starting your journey or looking to refine your routine, know that you have the power to manage your PCOS and live a vibrant, healthy life. You’ve got this—one step at a time!
read more on PCOS and fertility topics
